How Emotional Trauma Contributes to Chronic Pain
If you had asked me a year ago why my body hurt so much—why my hips ached, my calves tightened with every step, or why even walking on the treadmill felt like a chore—I would have said it was from overtraining or poor posture. What I couldn’t articulate then was that my pain wasn’t just physical. It was a complex dance involving my nervous system, my fascia, and my body’s attempt to protect itself after years of unresolved trauma.
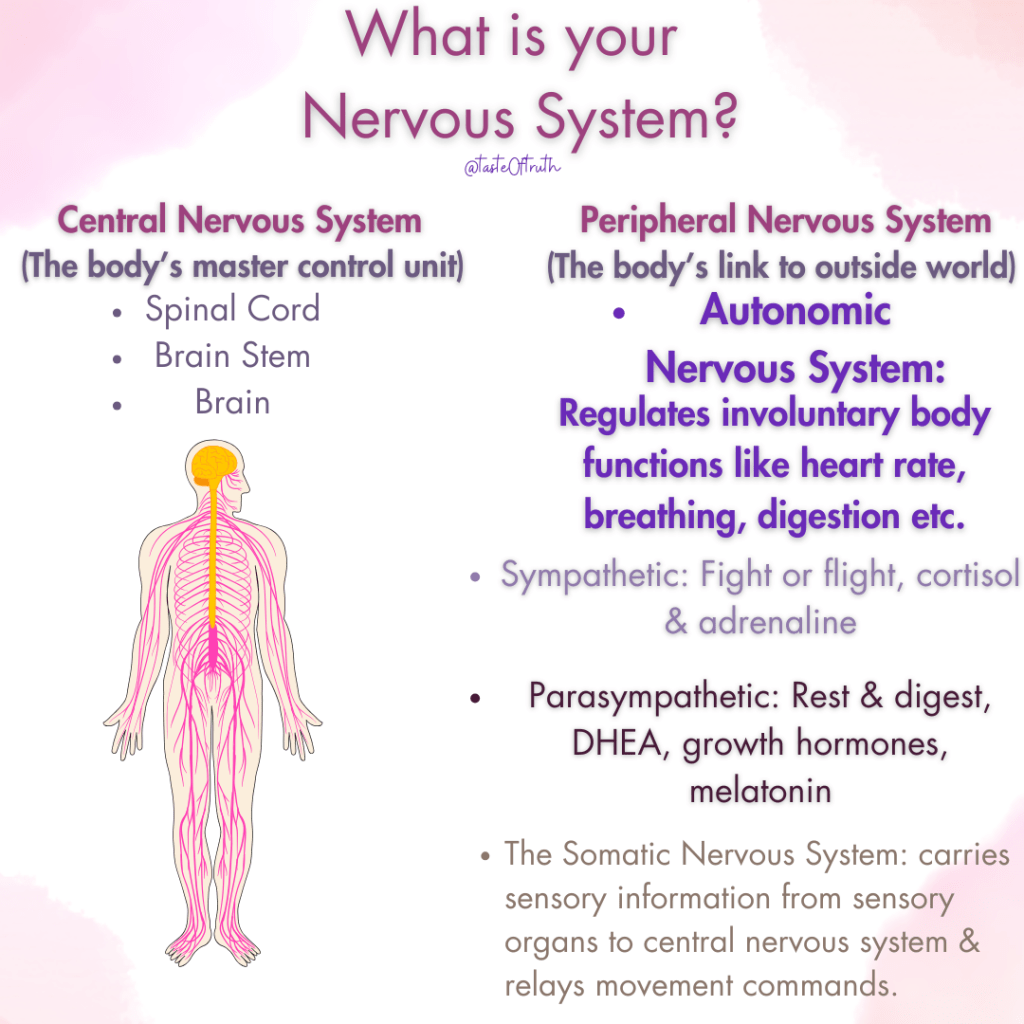
Our nervous system plays a fundamental role in chronic pain. When we experience physical or emotional trauma, our body reacts by creating a heightened state of alertness. Over time, these experiences are encoded in the nervous system as neurotags—clusters of physical, emotional, and cognitive memories that influence how we react to stress and pain. Chronic pain, I’ve learned, is often an echo of this activation. It’s not just about tight muscles or structural imbalances—it’s a survival mechanism trying to make sense of and respond to past trauma.
This is the story of how I’ve started to untangle it all, and how chronic pain, emotional wounds, and trauma are all intricately tied together in ways I never imagined.
The Connection Between Chronic Pain and Trauma
For years, I treated my body like a machine. During my bodybuilding days, I pushed through discomfort, ignored signs of overtraining, and celebrated soreness as a badge of honor. But what I didn’t understand then was how my nervous system was quietly keeping score.
Chronic pain, I’ve learned, isn’t just about tight muscles or structural imbalances—it’s a survival strategy. When we experience trauma, whether from overtraining, stress, or emotional wounds, our nervous system can get stuck in a heightened state of alertness. It’s like a smoke alarm that keeps going off, long after the fire has been extinguished.

Fascia, the connective tissue that surrounds every muscle and organ in our body, plays a fascinating role in this process. Fascia isn’t just structural—it’s sensory. It’s packed with nerve endings that communicate directly with the brain. When the body perceives danger (even subconsciously), the fascia can tighten, creating patterns of tension that mirror emotional or physical trauma. In my case, that tension showed up in my psoas muscles, my calves, and my lower back—all areas associated with safety and movement.
The more I explored these connections, the more I began to see that pain wasn’t random—it was a message from my body. And it was asking me to listen.

The Power of Neurotags: How Pain and Trauma Intersect
One of the most eye-opening concepts I’ve come across in my journey is the idea of neurotags—a term used to describe the brain’s way of organizing and processing sensory, emotional, and cognitive information. Neurotags are like maps of experiences that are built over time, creating an interconnected network of physical sensations, emotions, and thoughts that work together to form a response to stimuli.
Here’s the kicker: Chronic pain is often stored in these neurotags. When trauma occurs—whether physical, emotional, or psychological—it gets encoded in the nervous system as a pattern. These patterns are not just about the physical experience of pain, but also the emotions and thoughts tied to that experience.
When trauma is stored in the nervous system, it doesn’t just affect how we feel physically; it affects our entire emotional and cognitive landscape. For example, someone who has experienced physical trauma may also experience emotional flashbacks or cognitive distortions that are linked to that experience. These flashbacks are like sudden replays of past trauma, but they don’t just exist in the mind—they can show up physically in the body.
Neurotags, Emotional Flashbacks, and Chronic Pain
Think about it this way: When we experience a traumatic event, our nervous system reacts by encoding that event into a neurotag. This neurotag includes not only the physical sensations (like tightness, pain, or discomfort), but also the emotions (fear, anger, sadness) and cognitive patterns (thoughts like “I am unsafe” or “I am weak”).
Emotional flashbacks happen when the brain reactivates these neurotags, causing the body to respond as if the trauma is happening again. This is why someone with chronic pain may experience intense emotions that seem disproportionate to the physical sensations they’re feeling. The pain can trigger a flashback—a sudden, overwhelming re-experience of trauma that isn’t just mental but is felt deeply in the body.
In my case, the tension I experienced in my hips and lower back was a reflection of both the physical trauma of overtraining and the emotional trauma I had internalized from years of pushing myself too hard and ignoring my body’s signals. When my nervous system encountered stress, it activated these neurotags, making the tension and pain feel more intense and more pervasive. The more I resisted this pain or ignored the emotional connection to it, the worse it became.

How I’m Healing: Creating New Neurotags and Engaging the Vagus Nerve
Understanding neurotags has been revolutionary in how I approach my healing process. The key to healing, I’ve learned, is not simply “fixing” the physical pain but reprogramming the neurotags. This involves creating new patterns that support healing, safety, and relaxation.
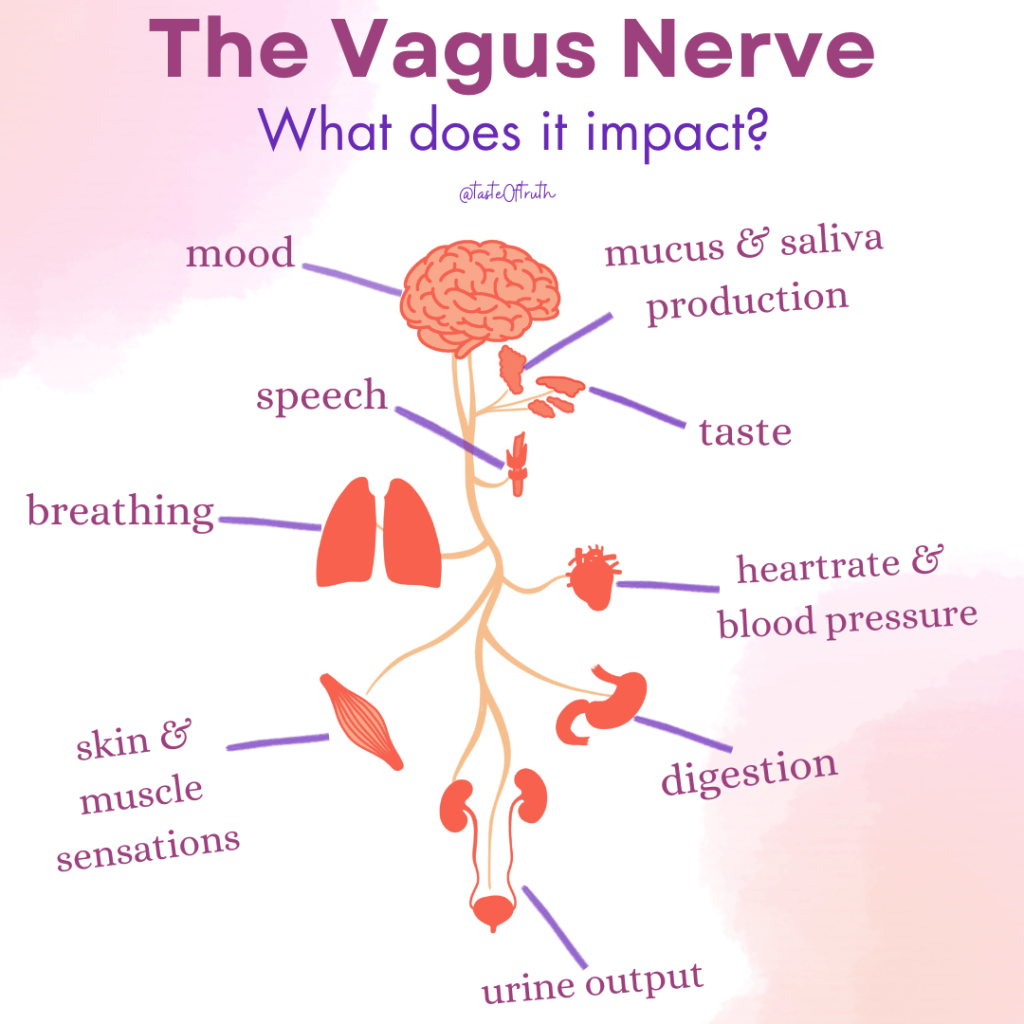
One powerful way I’m rewiring my nervous system is by engaging the vagus nerve, the longest cranial nerve that plays a critical role in regulating the parasympathetic nervous system. The vagus nerve is like the body’s “brakes,” helping to turn off the fight-or-flight response and return the body to a state of calm. When activated, it encourages relaxation, emotional regulation, and recovery—exactly what my body needs as I untangle the tension stored in my fascia and nervous system.
Here’s how I’m starting to rewire my system:
Reconnecting with Joyful Movement:
I’ve reintroduced activities that make me feel alive, like walking in the garden or playing with my pets. These moments remind me that movement isn’t just about strength—it’s about freedom. By incorporating joyful, non-stressful activities, I’m helping to reinforce new neurotags that associate movement with pleasure and ease.
Reclaiming Safety Through Movement:
Instead of high-intensity workouts, I’ve shifted to gentle, functional exercises that strengthen my core and glutes while supporting my nervous system. Slow, mindful movements like glute bridges, bird dogs, and pelvic tilts have become my new best friends. These exercises not only build strength but signal to my nervous system that it’s safe to move.
Releasing Fascia with Love:
I’ve embraced somatic practices like gentle rocking, diaphragmatic breathing, and fascia-focused stretches to help release tension. These practices aren’t just physical—they’re a way of telling my body, “You’re safe now.” They help reprogram the neurotags associated with stress and trauma by sending a message of relaxation and calm.
Vagus Nerve Activation:
To support my nervous system’s recovery, I’ve incorporated practices that stimulate the vagus nerve, such as slow, deep belly breathing and humming. Breathing deeply into my diaphragm (focusing on long exhales) has been especially helpful in calming my body and signaling to my nervous system that it’s okay to relax. By consciously engaging my vagus nerve, I’m helping shift from the fight-or-flight response into a restorative state.
Rewriting Emotional Patterns:
Rewiring my nervous system also means rewriting my emotional patterns. This involves acknowledging the emotional flashbacks that arise when pain triggers old neurotags and consciously choosing to respond with compassion and self-care. Instead of reacting with fear or frustration, I’m learning to pause, breathe, and remind myself that I’m safe now.

What Chronic Pain Has Taught Me
Chronic pain has been a tough teacher, but it’s taught me lessons I wouldn’t trade for anything:
- Your body is always on your side. Pain is a signal, not a punishment.
- Healing isn’t linear. Some days, progress looks like resting instead of pushing.
- Movement is medicine, but only when done with intention and love.
I share this journey because I know I’m not alone. So many of us carry the weight of trauma—both emotional and physical—in our bodies. And while the road to healing isn’t easy, it’s worth it.
If you’re navigating chronic pain, I want you to know this: Your body isn’t broken, and you don’t have to fight it. With the right tools, patience, and self-compassion, you can create safety, release tension, and rediscover the joy of movement.
I’m still on this journey, and I’d love to hear about yours. What has chronic pain taught you? How are you learning to trust your body again? Let’s keep this conversation going—because healing happens when we feel safe enough to share.